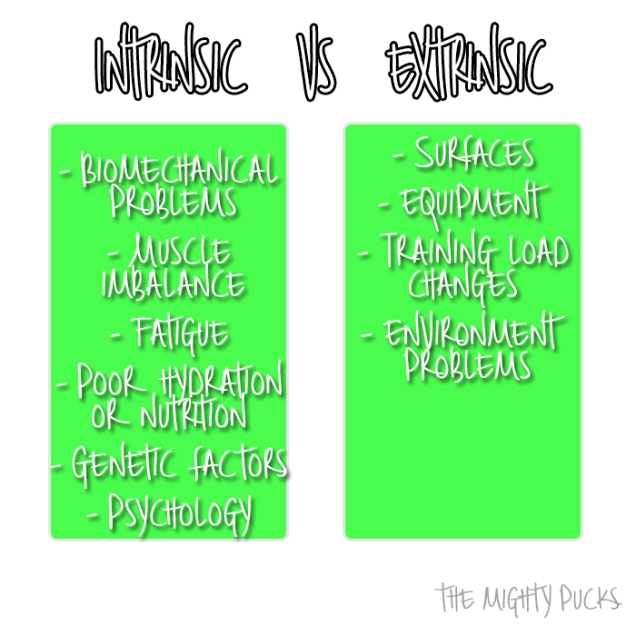
Considering that one of the NHL’s issues with the Olympics is potential injury risks to players, they sure do an absolutely horrendous job at managing safety throughout the league. Back when the Mighty Pucks was just starting, there were a series of posts about toxic masculinity in particular I wrote about playing through injuries being seen as a sign of manliness. The more “manly” a player perceives himself to be, the less likely he is to seek psychological treatment following significant injury, and although there are many reasons for playing on – including to benefit the team – in my personal view, one of the biggest road blocks is peoples’ attitudes.
NHLers are expected to be tough, to suffer through broken bones, stitches, busted teeth etc. They’re tough guys. They battle every night. They’re warriors, etc, etc, etc. It’s boring. Hockey culture has normalised playing on through injury to the point that players in the NBA are laughed at for leaving the court with sprains. Consider this: These are professional athletes whose income depends on their body’s ability to perform. It would take a lot of courage for a hockey player to say “you know what, I’ve done something to my ankle, I’m taking a couple of games off to rest”. However, say there are around 82 games in the regular season, NHL players have little time to recover from their knocks and if they took the time to fully recover, there’d likely be nobody in the roster. It’s been said that they can only really get to grips and heal in the off season and just “put up” with all their injuries.
Thank goodness that the San Jose Sharks have been knocked out in round one of the playoffs because Joe Thornton has been playing with a torn ACL and MCL. What did head coach Peter DeBoer have to say?
“I’ve never seen a guy play with a torn MCL and ACL… It’s a courageous effort as I’ve ever seen.”
Courageous?! It’s utterly ridiculous! His knee was floating! The man has torn two major ligaments in his knee. How the hell is he still moving around? Thornton, who is 37, had a 50 point season for the Sharks, and even in his four playoff appearances notched up two assists, however this was his lowest season since 98/99. The veteran player is a free agent this summer, so perhaps he was keen to show that he was still a valuable player. He has since undergone surgery for the tears with no timeline of return announced which leaves his future up in the air. A fellow veteran and teammate, 37 year old Patrick Marleau, is also an unrestricted free agent this summer. Like Thornton, he was also nursing a broken thumb during the post-season which will have affected his ability to shoot the damn puck.
There must be something in the water over in San Jose because a THIRD player has also been playing in the playoffs with an injury. Tomas Hertl had around 19 minutes of time on the ice during the playoffs despite having a broken foot. Not to mention that Logan Couture took a puck to the face towards the end of the regular season and said that it hurt to breathe. His bottom teeth were being held together by wires and the top had a plastic coating to stop them falling out. A member of the Sharks’ dental team explained that due to the freak deflection to Couture’s face, it was akin to him being hit with a large hammer. Nonetheless, Couture was back for the playoffs wearing a cage – risking taking another knock to the face. It is likely that he’ll need a good number of those teeth removed this summer now he has the opportunity to recover.
“In my mind, I wish I could have played right after it happened”
Is any of this making you ask “what the hell is going on in the NHL?” because I certainly ask that on a daily basis.
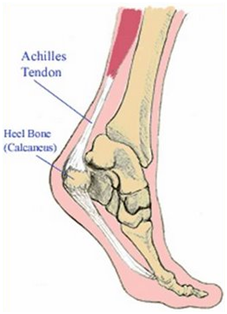
Zach Werenski attempted to block a shot and deflected a  puck into his face but returned to the game in the third period… however due to extreme facial swelling he did not play in overtime and was ruled out of the remainder of the Blue Jackets postseason. He was allowed to play until his face swelled so much! That’s not right! Erik Karlsson of the Ottawa Senators revealed that he’s been receiving injections in his heel because he’s skating on two hairline fractures. What’s scarier is that Karlsson leads in total time on ice during the playoffs with 182.23 minutes.
puck into his face but returned to the game in the third period… however due to extreme facial swelling he did not play in overtime and was ruled out of the remainder of the Blue Jackets postseason. He was allowed to play until his face swelled so much! That’s not right! Erik Karlsson of the Ottawa Senators revealed that he’s been receiving injections in his heel because he’s skating on two hairline fractures. What’s scarier is that Karlsson leads in total time on ice during the playoffs with 182.23 minutes.
These aren’t just rare superhuman feats found in this year’s playoffs… Back in 2014, the Penguins favourite Finn, Olli Maatta took two weeks out of the season to have surgery to remove a cancerous tumour from his thyroid. TWO WEEKS. Also in 2014, teammate Kris Letang, who was 26 at the time, suffered a stroke and took a lengthy six weeks out. Yeah, six whole weeks after suffering a stroke…
I understand that the majority of players in the playoffs are dealing with injuries and we only really find out the extent of them once the team is eliminated, but it is worrying how normal this is to them. Athletes have a very short “lifespan” as a pro and there’s a toss-up between sucking it up and continuing whilst hurt, risking further injury, or taking time away to actually heal and worry about coming back. To the owners of the league, the players are disposable. One of the biggest issues I have is that boys in general are taught from a very young age to be tough and not to cry when they’re hurt, and this seems to be a thousand times worse with hockey players. Granted, it’s a rough game, but there comes a point where toughness becomes a ridiculous rigid resilience where health is neglected and the players are congratulated for continuing to play with their limbs hanging off. Secondly, the NHL is terrible at enforcing safety throughout the league yet have the audacity to proclaim a big reason to not attend the Olympics is due to injury risk. For one thing, players rarely fight in the Olympics because they’re ejected from the game – and fighting increases your risk of injury without a doubt, yet still exists in the league. Then there is the lack of concussion prevention/support which is a huge issue in hockey, but the NHL is too busy lining their pockets than actually focussing on the player’s health.
The short version: Hockey players are applauded for suffering through injuries and continuing to play as a result of a toxic, normalised attitude, and the league is unlikely to do anything about this because players are replaceable cogs in the money making machine that is the National Hockey League.